Introduction
Referral of inquiry and terms of reference
1.1
The Select Committee into the Obesity Epidemic in Australia was
established on 16 May 2018. The committee is composed of seven Senators.
1.2
The committee is tasked with inquiring into and reporting on the
following terms of reference:
- The prevalence of overweight and
obesity among children in Australia and changes in these rates over time;
- The causes of the rise in
overweight and obesity in Australia;
- The short and long-term harm to
health associated with obesity, particularly in children in Australia;
- The short and long-term economic
burden of obesity, particularly related to obesity in children in Australia;
- The effectiveness of existing
policies and programs introduced by Australian governments to improve diets and
prevent childhood obesity;
- Evidence-based measures and
interventions to prevent and reverse childhood obesity, including experiences
from overseas jurisdictions;
- The role of the food industry in
contributing to poor diets and childhood obesity in Australia; and
- any other related matters.
1.3
This report is comprised of 10 chapters, as follows:
- This chapter (Chapter 1) provides some background information
around the prevalence of obesity, and defines some key terms;
- Chapter 2 discusses the importance of language and the high
degree of stigma attached to the term 'obesity';
- Chapter 3 examines strategic policy directions which could help
tackling obesity;
- Chapter 4 discusses the issue of food labelling;
- Chapter 5 focuses on the critical role of reformulation to
improve the availability of healthier products;
- Chapter 6 examines the benefits of introducing a tax on sugary
drinks;
- Chapter 7 focuses on the issues associated with the marketing and
advertising of discretionary foods;
- Chapter 8 discusses the importance of education campaigns;
- Chapter 9 looks at the benefits of health care interventions; and
- Chapter 10 discusses promising multi-strategy prevention programs
to prevent and address the prevalence of obesity at community level.
Conduct of the inquiry
1.4
The committee received 150 submissions to the inquiry from individuals
and organisations. These submissions are listed in Appendix 1.
1.5
The committee also conducted four public hearings:
- 06 August 2018 in Sydney;
- 07 August 2018 in Melbourne;
- 04 September 2018 in Melbourne; and
- 05 September 2018 in Melbourne.
1.6
Transcripts from these hearings, together with submissions and answers
to questions on notice are available on the committee's website. Witnesses who
appeared at the hearings are listed in Appendix 2.
Acknowledgments
1.7
The committee would like to thank the individuals and organisations that
made written submissions to the inquiry, as well as those who gave evidence at
the four public hearings. We are grateful for their time and expertise.
Note on terminology and references
1.8
References to submissions in this report are to individual submissions
received by the committee and published on the committee's website. References
to Committee Hansard are to official transcripts.
Definitions
1.9
The committee received evidence from a number of submitters on how to
define some of the terms used across the spectrum of issues covered by the
committee's terms of reference. Reaching an agreed definition on some of these
terms underpins an understanding of the problems faced, and helps focus
potential solutions.
1.10
The terms range from the technical definition of particular types of food,
to how overweight and obesity themselves are defined, right through to how
children are defined in relation to areas such as advertising.
Food
1.11
Discretionary foods were the subject of much discussion in evidence to
the inquiry. The Australian Beverages Council describes discretionary foods as:
...foods and drinks [that] are not necessary for a healthy diet
and are high in saturated fat and/or added sugars, added salt or alcohol and
low in fibre (22), e.g. alcohol, cakes, biscuits, confectionery, chocolate and
some non-alcoholic beverages.[1]
1.12
The Australian Bureau of Statistics (ABS) similarly cites the Australian
Dietary Guidelines' description of these foods as being non-essential, although
they may add variety and can still be consumed safely in small quantities
depending on one's lifestyle:
...foods and drinks not necessary to provide the nutrients the
body needs, but that may add variety. However, many of these are high in
saturated fats, sugars, salt and/or alcohol, and are therefore described as
energy dense. They can be included sometimes in small amounts by those who are
physically active, but are not a necessary part of the diet.[2]
1.13
While all sugar is processed by the body in the same way, sources of
that sugar determine how that sugar is treated in regard to dietary guidelines
and food preparation. Free sugars are those naturally present in food
substances such as honey and fruit juice, while 'added sugars' are those added
during the manufacture of food, and include 'sucrose, fructose, dextrose,
lactose and sugar syrups such as glucose syrup'.[3]
Body Mass Index (BMI)
1.14
The ABS describes the BMI as 'a simple index of weight-for-height that
is commonly used to classify underweight, normal weight, overweight and
obesity. It is calculated from height and weight information, using the formula
weight (kg) divided by the square of height (m)'.[4]
1.15
The limitations of BMI as the sole indicator of a healthy weight,
particularly in relation to children, were discussed by submitters throughout
the inquiry.[5]
Overweight and obesity
1.16
Overweight and obesity are defined as abnormal or excessive fat
accumulation that may impair health. For adults, the World Health Organisation
defines overweight as a BMI greater than or equal to 25; and obesity as a BMI
greater than or equal to 30.[6]
Children
1.17
For the purposes of this inquiry the definition of children is important
not only in terms of how to measure and assess a healthy weight, but it is
crucial in relation to how particular foods are marketed and advertised.
1.18
A number of perspectives around advertising and marketing aimed at
children were explored throughout the inquiry. TV advertising in particular
categorises its audience in terms of age, so how children are defined is
important in this context. This is further discussed in Chapter 2.
Background information
1.19
In Australia, rates of overweight and obesity have risen dramatically in
recent decades in all age groups, with the increase most marked among obese
adults.[7]
1.20
Overweight and obesity in adults and children is associated with
significant health impacts. Poor diets and high BMI are the major risk factors
contributing to Australia's disease burden, ahead of smoking-related illness.[8]
Prevalence of overweight and
obesity in Australian adults
1.21
In 2014–15, 63 per cent of Australian adults were overweight or obese. Seventy‑one per
cent of men were overweight or obese, compared with 56 per cent of women.[9]
1.22
Prevalence of overweight and obesity is higher for adults living outside
major cities. Sixty per cent of Australians in major cities are overweight or
obese, compared to 69 per cent in inner regional Australia and 70 per cent in
outer regional and remote Australia.[10]
1.23
For women, the prevalence of overweight and obesity varies according to
socioeconomic group. In 2014–15, about three in five women in the lowest
socioeconomic group were overweight or obese, compared with less than half of
those in the highest socioeconomic group. However, for men, prevalence of
overweight or obesity was similar across socioeconomic groups.[11]
1.24
In 2012–13, after adjusting for differences in age structure, Aboriginal
and Torres Strait Islander adults were 1.2 times as likely to be overweight or
obese as non‑Indigenous adults, and 1.6 times as likely to be obese.[12]
International comparisons
1.25
Among 22 Organisation for Economic Co-operation and Development countries,
more than half (57 per cent) of people aged 15 and over are overweight or obese
(based on data for 2016 or the closest available year). Of those countries,
Australia's obesity rate (28 per cent of the population aged 15 and over) was
the 5th highest, behind the United States of America (38 per cent), Mexico (33
per cent), New Zealand (32 per cent), and Hungary (30 per cent), and was
higher than the 23 per cent average rate.[13]
Graph 1.1—Proportion of
overweight and obese by country
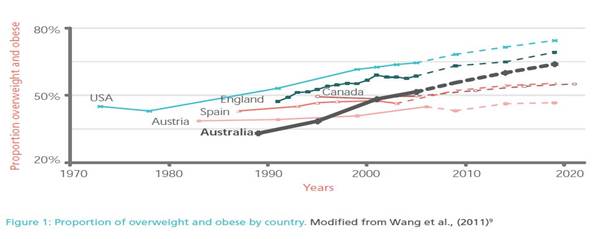
Source: Obesity Australia, Obesity: A national epidemic and
its impact on Australia, 2014, p. 7.
Prevalence of overweight and
obesity in children
1.26
Over the past 40 years, the prevalence of overweight and obesity among
Australian children increased at an alarming rate (see graph 1.2).
Graph
1.2—Prevalence of overweight and obesity among Australian children from 1969 to
2014-2015
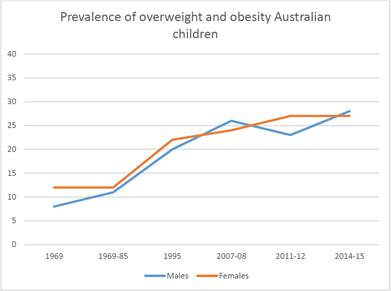
Source: Australian Health Policy Collaboration, Submission 59, p. 6.
1.27
There are currently over one million children in Australia who are
overweight or obese.[14]
1.28
In 2014–15, 20 per cent of children aged 2–4 were overweight or obese—11
per cent were overweight, and 9 per cent were obese. Twenty-seven per cent of children
and adolescents aged 5–17 were overweight or obese—20 per cent were overweight,
and 7 per cent were obese. For both children aged 2–4 and 5–17 years, similar
proportions of girls and boys were obese.[15]
1.29
Aboriginal and Torres Strait Islander children and adolescents are more
likely to be overweight or obese than non-Indigenous children and adolescents.
In 2012–13, 30 per cent of Aboriginal And Torres Strait Islander children and
adolescents aged 2–14 were overweight or obese, compared with 25 per cent of
their non-Indigenous counterparts.[16]
International comparisons
1.30
The prevalence of infant, childhood and adolescent obesity is rising
around the world. Although rates may be plateauing in some settings, in
absolute numbers there are more children who are overweight and obese in low and
middle-income countries than in high-income countries.[17]
Short and long-term harm to health
associated with obesity
1.31
The link between obesity and poor health outcomes is well established.
Overweight and obesity lead to heightened risk of developing chronic diseases,
including cardiovascular disease and type 2 diabetes. In particular, visceral
fat, which is stored around the body's vital organs, has been associated with
increased risk of heart disease and metabolic disorders.[18] Being overweight or obese also increases risk for at least 13 types of cancer,
including breast and colon cancer.[19]
Childhood Obesity
1.32
Overall, children with overweight and obesity are more likely to
experience poorer health status and lower emotional functioning.[20]
1.33
Children's and adolescents' short-term health impacts include chronic
conditions such as breathing difficulties, fractures, hypertension, insulin
resistance and early markers of cardiovascular disease.
1.34
The most significant long-term health impacts of childhood obesity that
manifest in adulthood are cardiovascular disease, diabetes, musculoskeletal
disorders (osteoarthritis), and certain types of cancer (endometrial, breast
and colon).[21]
1.35
Many submitters and witnesses focussed strongly on how childhood obesity
can be prevented, given the serious implications all through life that being
overweight or obese in childhood brings.
1.36
In purely economic terms, the committee heard that early intervention is
the key to preventing higher healthcare costs. Dr Shirley Alexander from The
Children's Hospital Westmead told the committee:
[R]aising the issue to enable early intervention for greater
success. Research indicates that healthcare costs for children with obesity,
even as young as between two and five years of age, are much higher than those
for children of a healthy weight. Interventions using family-centred
behavioural change in diet and activity have been shown to be effective. [22]
1.37
In health terms, the picture is similarly bleak:
Worryingly, the prevalence of severe obesity in the
paediatric population has increased significantly, to the point that we [are] now
see children as young as eight years old with type 2 diabetes.[23]
1.38
The overall impact of obesity on a person's life course was also
discussed by a number of witnesses. Dr Nicole Black from the Centre for Health
Economics at Monash University cited research showing the pervasive reach of
the obesity:
There's been quite a lot of research looking at the health
consequences of childhood obesity as well as the psychosocial and developmental
consequences during childhood. We know that these consequences can affect
children over their whole life course. There's evidence suggesting that, for
example, obesity in children is likely to lead to more emotional problems and
it's likely to lead to more social problems during school. Other research has
shown that these problems can lead to problems in academic achievement, it can
affect their educational attainment and it can affect their employment
prospects later in life. We've also got evidence from studies that look at the
social and economic impacts of adolescent obesity. As these adolescents enter
adulthood, if they were obese during adolescence they're less likely to be
married, for example, and they're less likely to have a high household income
than adolescents who were of normal weight.[24]
1.39
The grave concerns are supported by Mrs Belinda Smith from The Root
Cause, an organisation that focuses on children making healthier food
choices. Mrs Smith outlined the misconceptions around what children will
eat, and the consequences of this lack of understanding:
There's also a frightening lack of understanding amongst many
parents and children about the impact these foods are having on health,
behaviour, concentration and academic results. Sadly, we are growing a
generation of children who are likely to go into adulthood with expensive
chronic illness such as fatty liver disease, type 2 diabetes, heart disease and
obesity, and neurological disorders like dementia and mental illness.[25]
1.40
Dr Seema Mihrshahi from the Centre of Research Excellence in the Early
Prevention of Obesity in Childhood outlined many of the factors that influence
whether children will become overweight or obese in their early years:
So it's not just caused by the imbalance of intake and
expenditure; there are a multiple levels of influence. With little children
it's also the family level influences: the availability of healthy food;
mothers breastfeeding; parents' preferences and modelling; physical activity;
and the knowledge, education and skills of the parents. Then there are the
community level influences, such as parks and green space around for parents to
take their children to, and cycle ways and cycle paths. Then there are the government
and societal influences: government policies, marketing of unhealthy foods to
children and so forth. So it's those societal influences that have really
changed over the last 20 years.[26]
Navigation: Previous Page | Contents | Next Page